Empower Health Plans to Optimize Risk, Revenue & Compliance
Unlock compliant risk adjustment, reduce denials, and drive sustainable growth with AI designed for payers.
Health plans lose $20B+ annually to coding inaccuracies, compliance audits, and preventable claim denials. Carevyn equips payers with AI-powered automation that strengthens compliance, improves risk adjustment, and accelerates revenue integrity.
 Payer-Focused
Payer-FocusedTransforming Payer Operations with AI
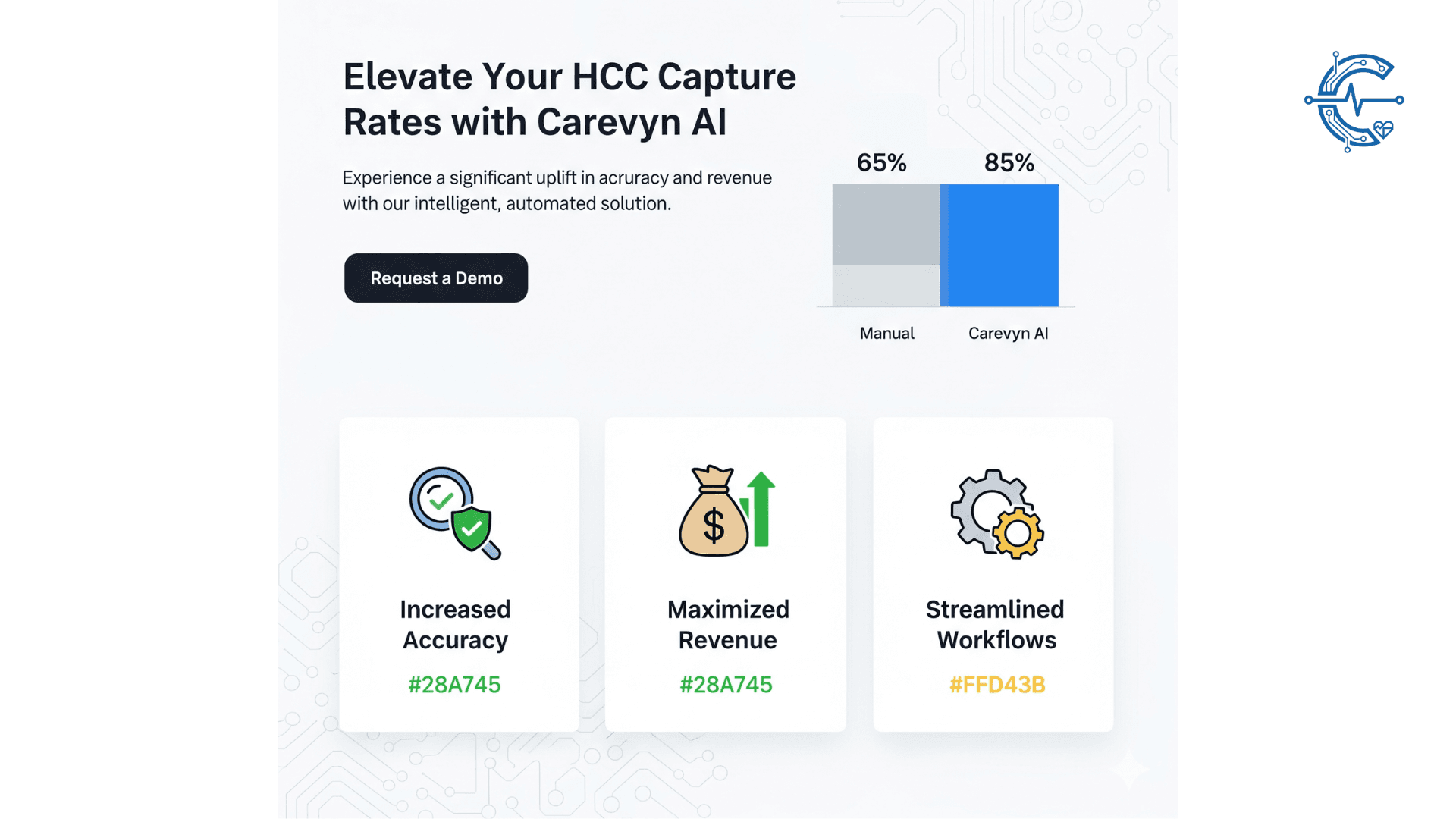
Evidence-Backed Risk Adjustment
- ✓95%+ coding compliance with AI-powered audit-ready documentation
- ✓20% higher HCC capture rates
- ✓Millions saved in avoided CMS penalties and clawbacks
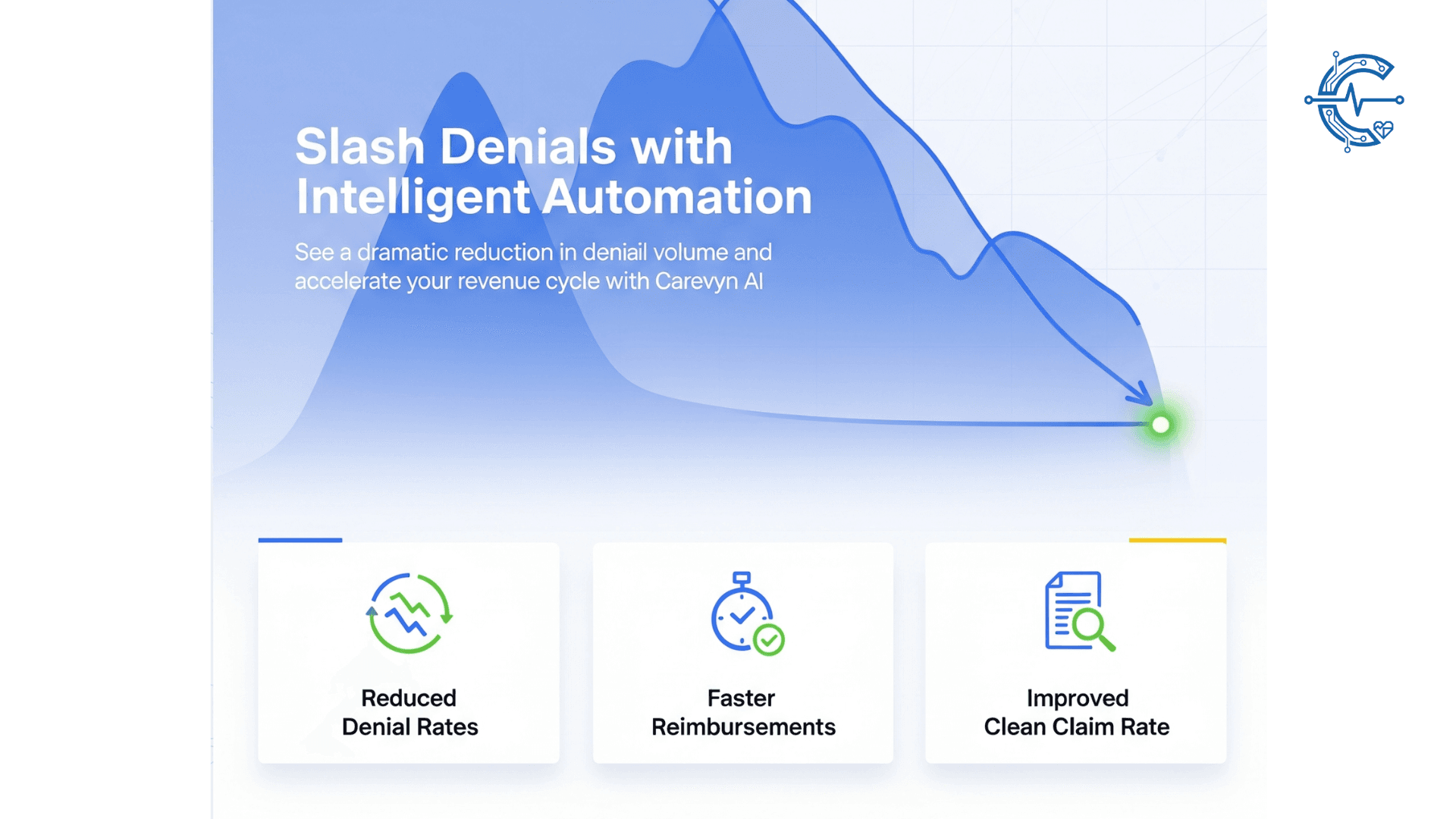
Reducing Denials & Enhancing Claims Integrity
- ✓25–30% reduction in preventable denials
- ✓15% faster claims resolution
- ✓Improved provider satisfaction through cleaner submissions
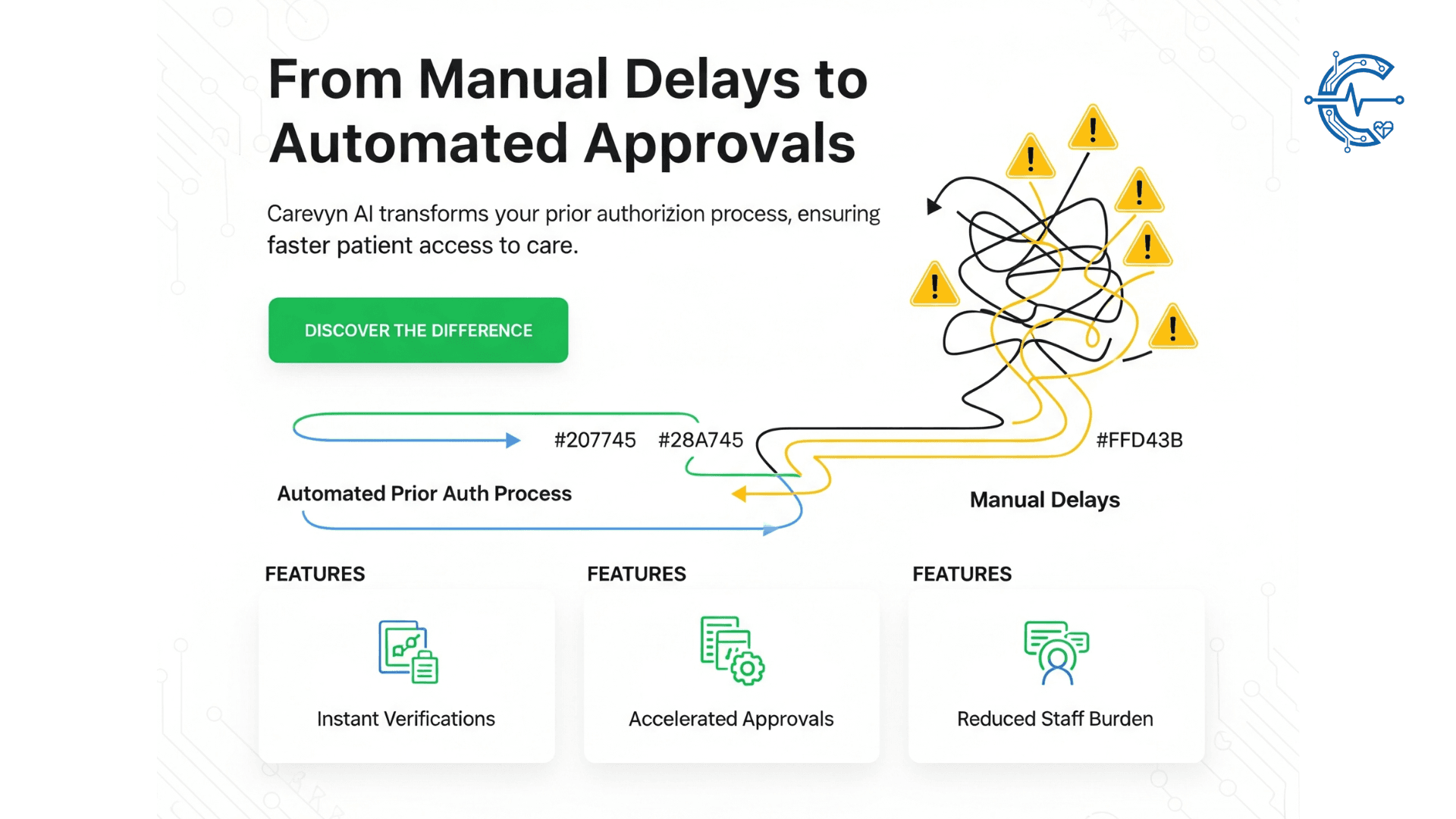
Real-Time Prior Authorization & Eligibility
- ✓70% faster authorization approvals
- ✓Automated eligibility checks to reduce backlogs
- ✓Improved member experience with quicker access to care
Supporting Value-Based Reimbursement Models
- ✓20% better alignment of risk scores with member health
- ✓15% increase in reimbursements tied to accurate coding
- ✓10% lower costs through predictive care management insights
Seamless Payer Platform Integrations
Carevyn connects seamlessly with payer systems, enabling health plans to optimize risk adjustment, reduce denials, and improve member outcomes through intelligent automation.
Payer Integration Capabilities
- ✓Integrates with major payer systems and clearinghouses
- ✓HIPAA-compliant, SOC 2 certified security
- ✓Real-time data exchange with provider networks
- ✓Scalable across multi-state health plans
- ✓Automated HCC capture and risk adjustment workflows
- ✓Real-time claims processing and denial prevention
"Achieve 95%+ coding compliance while reducing manual review by 70%."
Why Health Plans Choose Carevyn
95%+ Coding Compliance
Audit-ready risk adjustment with AI-powered documentation.
30% Fewer Denials
Reduce leakage and boost revenue with cleaner claims.
70% Faster Prior Auth
Accelerate member care access with real-time automation.
20% Higher HCC Capture
Optimize value-based contracts and risk adjustment.
Secure, Scalable, Trusted
SOC 2 + HIPAA certified, trusted by national payers.
Ready to Optimize Your Health Plan?
Carevyn enables health plans to streamline compliance, maximize reimbursements, and support member care with intelligent automation.